CHWs Changing Outcomes in South Carolina
Overview
Over the last decade, the refocusing of healthcare to quality- and outcome-based approaches has demonstrated a myriad of positive outcomes – particularly those related to returns on investment and improvements in patients’ health. Though these types of approaches are becoming more recognized, the transition has been a slow and inconsistent one. In the meantime, healthcare costs continue to rise, and health disparities remain apparent. South Carolina is not excluded from these changes and challenges. While addressing these issues is complex, there are evidence-based approaches that the state is in a prime position to begin implementing. One such approach involves the employment of community health workers (CHWs).
As the evidence demonstrating the impact CHWs have on health outcomes and spending continues to expand, we must intentionally move toward sustainable ways to support this critical workforce. Currently, CHWs in South Carolina are mainly funded by “program” or “project” grants and contracts that are often short term, subject to appropriations or private philanthropic decisions, and focused on specific, time-limited goals[1].
For South Carolina’s residents to reap the benefits and cost savings of CHWs employed at their full capacity, we need a budgeting mechanism for CHW positions that is not dependent on applying for grants, and that creates stability and sustainability for these programs throughout South Carolina.


James R. Clark Memorial Sickle Cell Foundation
Project Goals
Following initial funding from the South Carolina General Assembly, this initiative has been renewed for a third year with funding provided by the South Carolina Department of Health and Human Services to support an expanded focus on addressing existing health inequities in our state and reducing cost of care through the creation of a Community Health Worker (CHW) Pilot Program. Funding for this pilot is being implemented by the Center for Community Health Alignment (CCHA) with evaluation conducted by the Center for Rural and Primary Healthcare (CRPH). CCHA has partnered with organizations across the state to improve the health of underserved individuals in South Carolina through Community Health Workers (CHWs).
In alignment with yearly project goals, we also also currently have a five-year plan which encompasses two more years of the pilot complemented by proposed policy changes that allow for the expansion and sustainability of CHW services. Click on the bars below to learn more about the goals for each year.
Year 1
In Year 1 (2021-2022), the pilot funded twenty-one (21) CHWs across 12 organizations located statewide, as well as three additional technical assistance providers. CCHA identified and selected these sites, provided ongoing technical assistance to support effective CHW models and data collection, oversaw project implementation, and coordinated communication between administrative and participating entities.
Data captured in the initial 1-year period reflected over 2,500 patients served through nearly 5,000 separate encounters. CHWs provided a range of services, including, but not limited to: application assistance, referrals to support identified social determinants of health, vaccine scheduling, patient advocacy, community and patient relationship building, and health education. The first annual report was provided by the CRPH evaluation team in early 2023.
Year 2
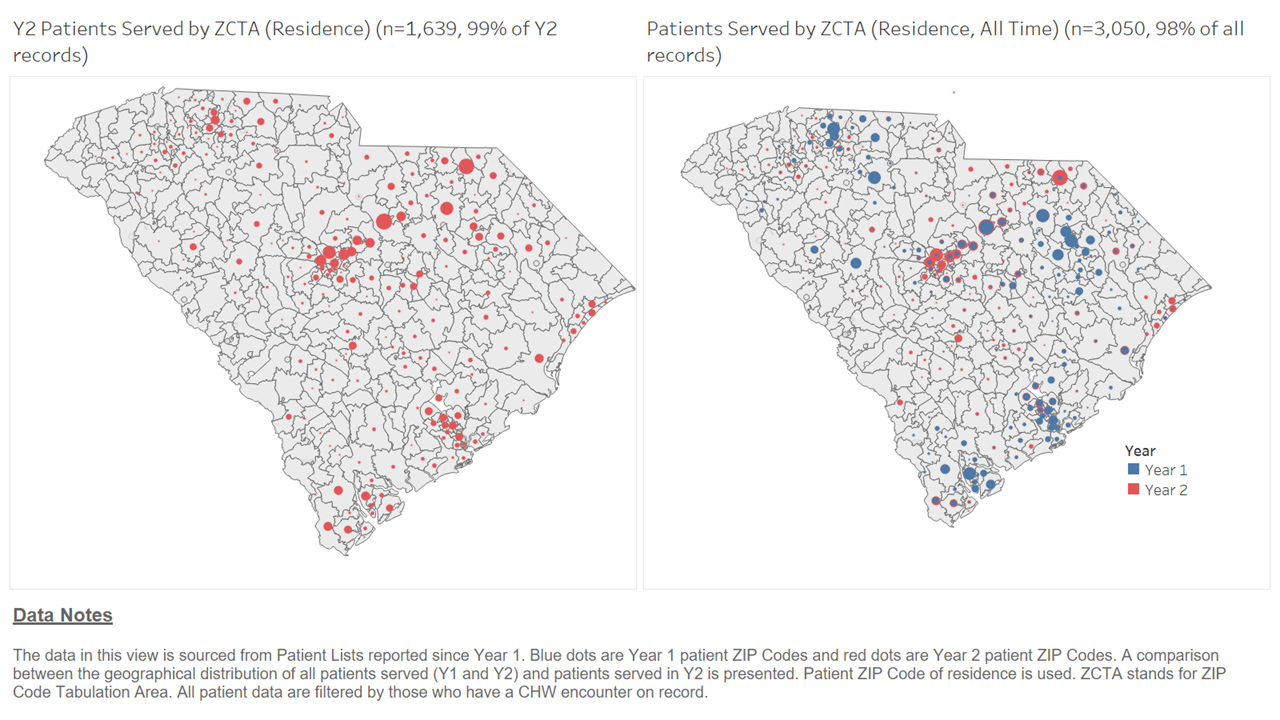
Year 2 (2022-2023) data collection continued through October 31st, 2023. Alongside the addition of a new health topic, perinatal health, twenty-three (23) CHWs from 14 community organization partners will help improve the health of South Carolinians, with coverage in all 46 counties.
CCHA maintained the same roles as in year 1, with the addition of assuming administrative responsibilities. CCHA and CRPH will support partners in continuing to demonstrate the ongoing, day-to-day impact of CHWs; corresponding data collected during the pilot period is expected to translate to improved long-term health outcomes and decreased medical spending.
To align with shifts in partner focus as well as project-wide revised priorities for data and reporting, year 2 also saw the addition of the perinatal health topic as well as discontinuation of the immunizations topic.
Year 3
Year 3 (2023-2024) is currently in progress, with 19 CHWs from 12 organizations across the state participating. Key results obtained from annual and quarterly reports to date are included below. To more accurately capture the day-to-day impact of CHWs, evaluation processes for year 3 have shifted to prioritize referrals, CHW core roles/services, needs identified, and needs addressed in addition to existing indicators.
In year 3, the pediatric asthma topic was also discontinued.
Our Approach
Requirements
For each funding year to date, partner organizations have submitted an online proposal detailing their scope of work, reporting capabilities, and other program-related details.
In alignment with efforts to support and advance the CHW workforce, CCHA requires that CHWs Changing Outcomes in SC partners provide a payment rate equivalent to at least $18/hour for all participating CHWs. CCHA encourages partners to establish equitable pay for CHWs and to support CHW certification and CHW career growth. Accordingly, CCHA’s training opportunities in CHW Core Competencies and CHW Specialty Tracks are currently offered free of charge to participating CHWs.
Partners must also submit quarterly reports with requested data. As needed, technical assistance (TA) around data and reporting, as well as other topics related to recognized best practices for CHWs, is provided by CCHA.
Additionally, PASOs and the South Carolina Hospital Association also serve as TA providers for participating PASOs affiliates and AccessHealth Networks, respectively.
Evaluation
Quantitative evaluation of partner-submitted quarterly reports is conducted by CRPH. Qualitative evaluation, which includes processes such as in-depth interviews with CHWs, photovoice, sharing of success stories, and other approaches, is conducted by CCHA. Both quantitative and qualitative evaluation findings are compiled to illustrate not only the resulting impact of CHWs, but also the unique skills, characteristics, and context—the “how”—behind that impact.
Priority Health Topics
At the start of the Year 2, participating organizations chose to focus on one or more of the following priority health topics most relevant to the needs of the communities they serve:
- Diabetes (Type II)
- High Need/High-Cost Service Use
- Perinatal Health
- Sickle Cell Disease
Organizations were encouraged to select topics that aligned with their existing CHW workflows. Thanks to continued pilot funding, the Perinatal Health topic was included beginning in the Year 2 project scope.
General Indicators
Data to be collected across sites as appropriate include, but are not limited to:
- Number of individuals reached
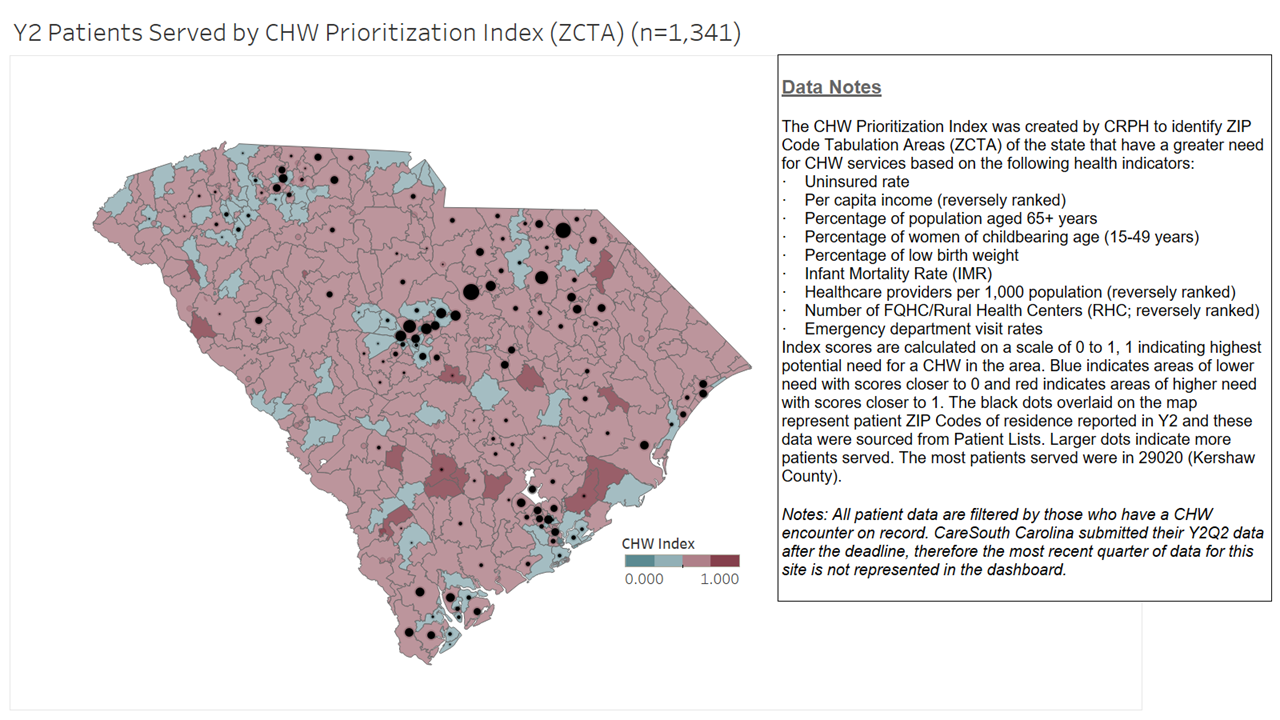
- Zip code of individuals’ residence
- Needs identified in screening
- Needs addressed
- Core roles/services provided by CHWs per patient encounter
- Patient demographics
- Referrals to health and social resources
- Medicaid claims data
Additional data specific to each selected health topic is also being collected.
Expected 2-Year Outcomes
- Increased number of individuals served in underserved areas of the state
- Increased access to social and health resources through community referrals and follow-up
- Increased access to care for individuals with Sickle Cell Disease
- Increased utilization of primary and preventive services by individuals with Type II diabetes and high need/high-cost healthcare utilization
- Increased access to perinatal health services and resources

Reach and Results
In the tabs below, examples of both qualitative and quantitative results from the initiative are shared.
Quantitative Examples of CHW Impact
From November 1, 2021, through the end of Q2 of Year 3 (April 30, 2024), CHWs participating in CHWs Changing Outcomes in SC have served 5,070 unique individuals through over 18,700 encounters.
Overview of Total Reach to Date (Year 1 through Q2 of Year 3)
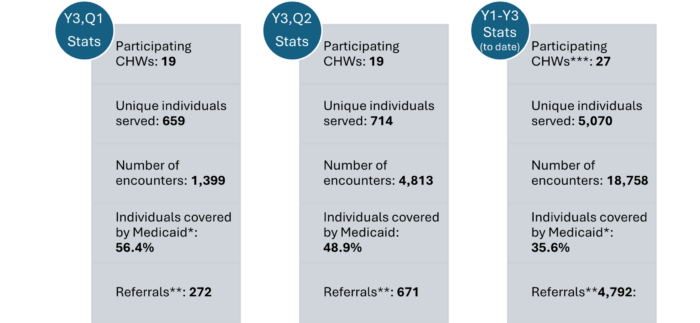
*Medicaid coverage information includes only participants for whom demographic information was reported.
**Referral closure loops were not reported consistently during Q1 due to reporting transitions. This information in Q2 reflects the referrals with a status reported (closed, open, client did not follow up).
***Indicates total number of CHWs who have contributed to the project data from Year 1 to present.
One major CHW role is addressing social determinants of health and access to care through linkages to services. In Q2, referral closure outcomes were reports for 547 referral records and 55% were closed-loop referrals, meaning that the individual received the service they needed. Further, for sites focusing primarily on addressing social determinants of health, 93% of referrals with closure outcomes indicated resulted in the corresponding service being received. This result is important because for most clinical providers or health systems, only the referral is measured (without the closing of the “loop”), meaning that it cannot be determined if the person indeed got what they needed.
Qualitative Examples of CHW Impact
For additional details, please see the two-pagers linked below.
Example 1: At Beaufort Jasper Hampton Comprehensive Health Services (an FQHC), a provider asked the CHW if she was available to work on a weekend. The CHW thought it was for a health fair, but the provider said it was for a patient she was trying to keep out of the hospital who needed a home visit to check on blood pressure. The CHW coordinated the home visit, reviewed medications with the patient, and found out the patient didn’t have a beta blocker. The CHW then notified the provider, who sent in a prescription that day; the patient picked it up next day, which the CHW confirmed when she returned to the patient’s home. By the patient’s follow-up on Tuesday, their blood pressure (BP) was excellent.
Example 2: At James R. Clark Memorial Sickle Cell Foundation (JR Clark), CHWs spend time helping individuals living with sickle cell disease (SCD) with their utility bills when they are struggling to pay them. For individuals living with SCD, extreme high or low temperatures can trigger SCD crises, which in turn results in greater usage of emergency medical services5,6. Additionally, stress can lead to SCD crises5 . While SCD is recognized as a progressive, lifelong disease, CHWs at JR Clark help patients avoid preventable emergency care usage by reducing both exposure to extreme temperatures and financial stress through providing support with utilities.
Example 3: A CHW at AccessHealth Tri-County highlighted how they effectively collaborate with physicians as a member of the patient’s care team. The CHW provides critical supports for the patient, such as helping to make medical information easy to understand and serving as a patient-provider liaison:
‘A lot of my patients… go to the free clinics and I work with the physicians that are there…the patient will see them usually once every [month]. And so…[the physicians] leave notes for me, and I leave notes for them. So i [the patient] saw their endocrinologist and I’m not able to [attend the appointment], I have the notes of what
was said or happened, if any medications change …when I meet with the patient I can further explain, ‘This is the
kind of medication you’re on. This is how you’re supposed to take it. How are you feeling?’ and things like that. Because patients don’t always understand the doctors, honestly… so that opens a door for me because they’re more trusting in me to say…’lt’s making me feel weird or it’s making me not have an appetite,’ or things like that. And so I can relate, I’m like that liaison, I can relay that to the physician, things that the patient doesn’t always feel comfortable saying. Because again, the theme that I do see is a lot of our…underinsured or uninsured [patients} …don’t feel like they have the right to question what their medical provider says when that is absolutely not the case.”
Example 4: Access Kershaw’s CHW connects patients to cancer screenings by collaborating with both providers and local and state resources, in addition to addressing social determinants of health-related needs. The CHW shared an example of a client that was able to receive a life-saving procedure for breast cancer:
“I had a former client come to me needing help getting medicine. She was having a hard time getting to her local FQHC. So after sitting there and talking to her about what was going on … I referred her to CareSouth. At the end of the appointment, the provider asked … ‘Is there anything else you have going on?’ And the client says, ‘Well, I had this lump on my breast.’ The provider turned around. She’s like, “I can see it from here…” [The client had} had this for some time….[a previous] provider [had} said …’you just have dense breasts.’ So [the client] went and had a mammogram. Turns out she did have cancer. CareSouth referred her to McLeod, and she started seeing McLeod, got a double mastectomy. But you know, the good news is, had I not referred her to them and they took care of her and got her connected to McLeod, this patient would not be here.”
The Upstate Family Resource Center

Beaufort-Jasper- Hampton Comprehensive Health Services
Partnerships and CHW Coverage
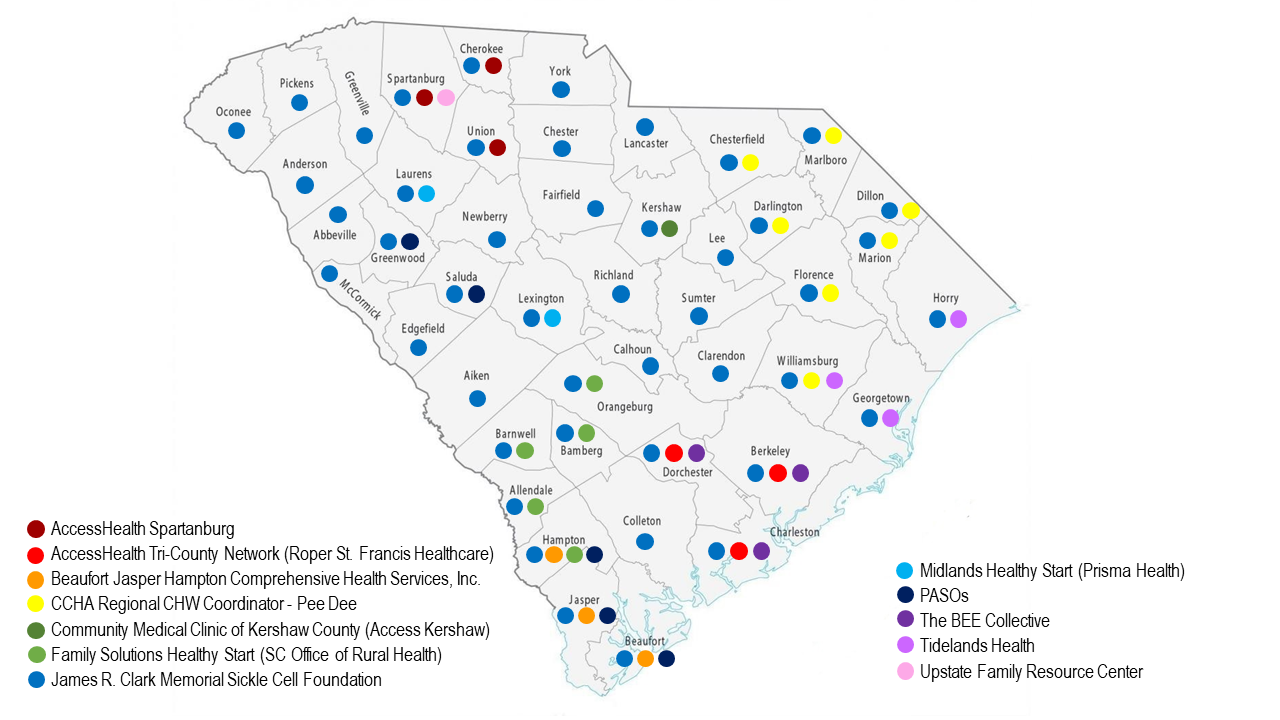
*Additional partners not listed on CHW coverage map:
- The Center for Rural and Primary Healthcare (CRPH; evaluation services, Year 1-present)
- The South Carolina Hospital Association (SCHA; technical assistance provider for AccessHealth sites, Year 1-present)
[1] Rush C. (2018) Sustainable Financing of Community Health Worker Employment. National Association of Community Health Workers. https://nachw.org/wp-content/uploads/2020/10/SustainableFinancingReportOctober2020.pdf
