Center for Community Health Alignment
Welcome to CCHA
We partner with community leaders to support health in underserved communities in South Carolina, regionally, and nationally.
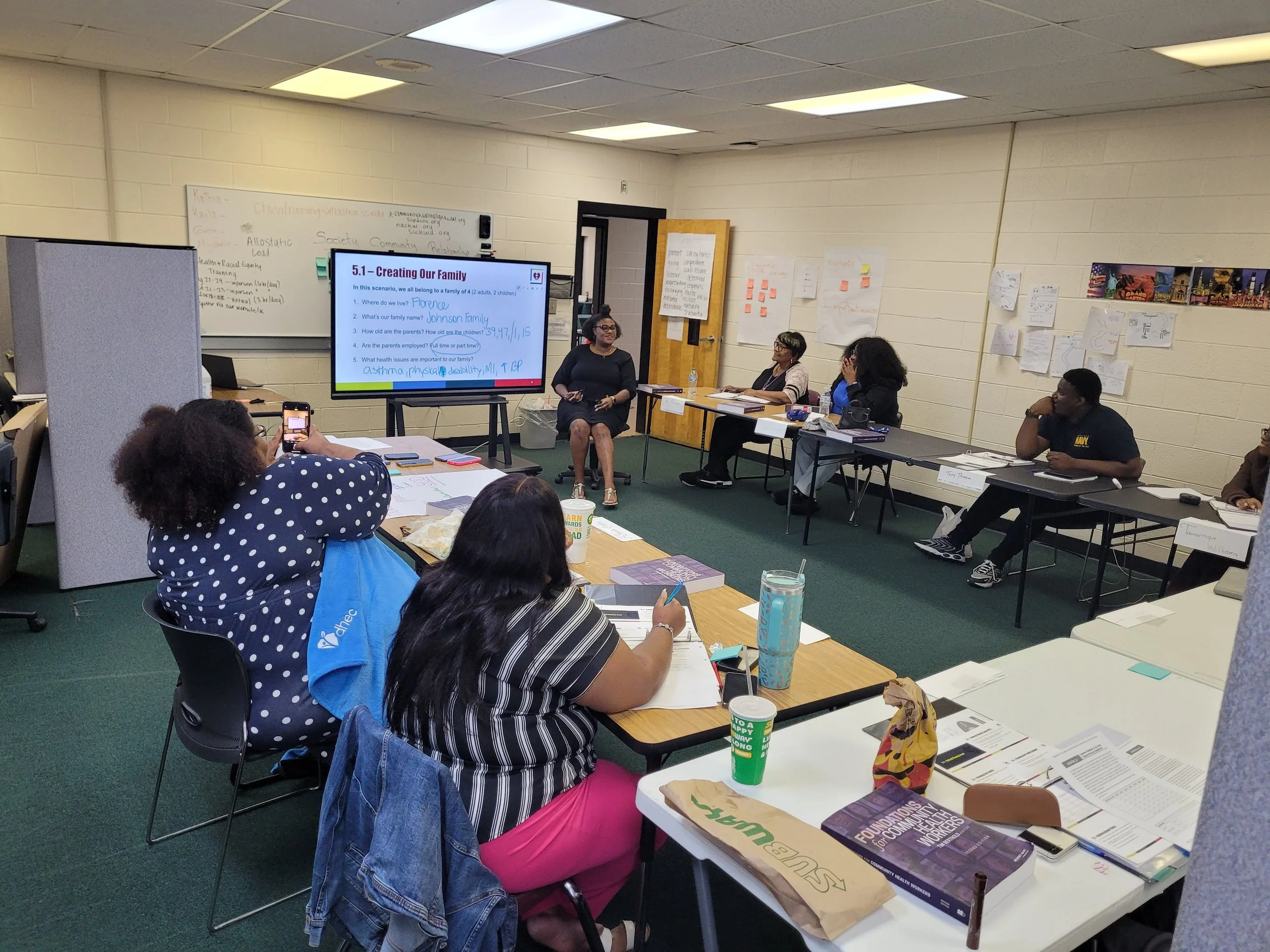
Since 2019, we have worked to create a strong CHW workforce through training, technical assistance, and program implementation.
Technical Assistance
TA supports the design, implementation, and expansion of CHW programs.
Training
Learn more about all trainings offered by CCHA for individuals and programs.
Our impact at a glance
Our training and technical assistance grow local capacity, improve access, and support measurable results.
393
CHWs Trained
in 2025
66
Organizations Supported with
TA or Capacity Building in 2025
$4.8 million
invested directly in CHWs to support their communities